News | COMPLEX PCI 2023
Precision in Stent Sizing: Insights from Imaging-Guided LM PCI
Emphasizing the Importance of Translating Scientific Numbers into Meaningful Clinical Insights

Jung-Min Ahn
Asan Medical Center, Republic of Korea
Dr. Jung-Min Ahn of Asan Medical Center, Korea, delivered an enlightening study on Left Main (LM) percutaneous coronary intervention (PCI), focusing on optimizing two-stent techniques for LM bifurcation stenting, especially in the Left Anterior Descending (LAD) and Left Circumflex (LCX) arteries.
Delving into the challenge of determining significant LM disease, Dr. Ahn highlighted the difficulty in measuring fractional flow reserve (FFR), particularly in cases involving distal downstream disease. His research demonstrated a significant correlation between the minimum lumen area (MLA) in the LM and FFR values. An MLA less than 4.5 showed a high positive predictive value for FFR values less than 80, providing a potential criterion for identifying functionally significant disease.
Dr. Ahn's research contributes significantly to the field, considering the default strategy for treating bifurcation lesions in Left Main Coronary Artery Disease (LMCAD) has been a simple crossover from the LM to the LAD artery. However, instances where two-stenting cannot be avoided were noted. The ongoing debate on provisional versus two-stent techniques, as seen in trials like DK-CRUSH V and EBC-MAIN, emphasized the need for clearer criteria, especially as a substantial proportion of patients initially categorized for provisional stenting end up receiving two stents.
The necessity for this approach is evident from various trials on LMCAD, including PRECOMBAT, EXCEL, and NOBLE, where a significant proportion of patients received two-stent techniques. Even in the EBC-MAIN trial, which generally favored one stenting, about 22% of patients in the provisional stenting group ended up receiving two stents, underscoring the importance of understanding how to optimize the two-stent technique for better clinical outcomes.
Addressing the ambiguity in defining when to choose between the two techniques, Dr. Ahn discussed the current lack of definitive criteria. While angiographic criteria have been suggested, the absence of Intravascular Ultrasound (IVUS) criteria remains a gap. He proposed integrating IVUS criteria into decision-making processes, referencing studies indicating the predictive value of minimal lumen area and plaque burden for functional outcomes.
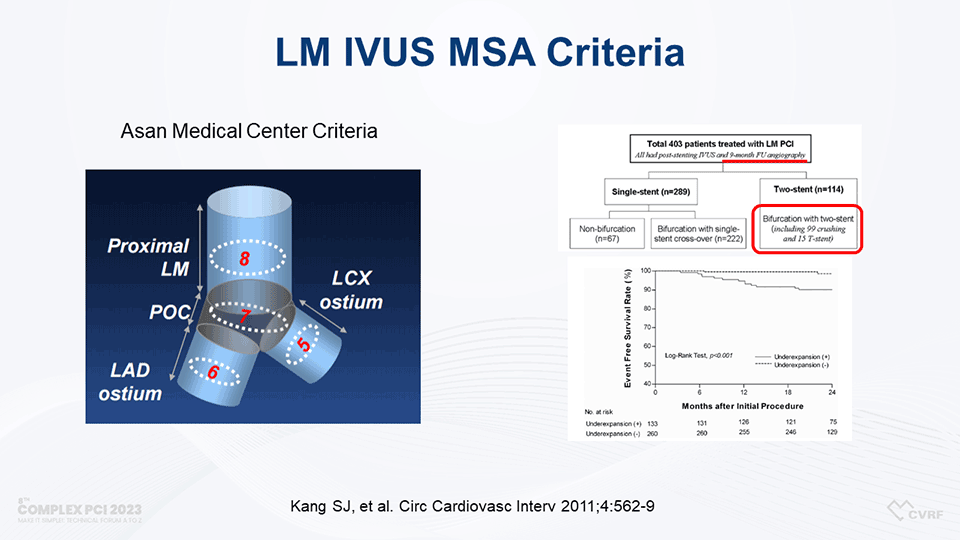
Dr. Ahn revisited the criteria established by Kang in 2011 while exploring the optimization of two-stent techniques. Kang et al. (2011) reported on minimal stent area (MSA) criteria for LM intravascular ultrasound (IVUS) from a diverse group of 403 patients undergoing LM PCI. However, the study's heterogeneity called for more specific MSA criteria, particularly concerning the LM crush technique. It's noteworthy that the EXCEL trial suggested a larger MSA compared to the established LM IVUS MSA criteria.
Emphasizing the necessity of refining these criteria, especially considering the heterogeneity of various stenting techniques, Dr. Ahn's recent analysis indicated that achieving larger minimum stent areas, particularly in the complex ostium of the Left Main, correlates with improved long-term outcomes. These findings offer potential benchmarks for optimizing stent size and contribute to the ongoing discussion on refining criteria for LM PCI.
The lecture provided insights into the ongoing debate about event rates between simple crossover and two-stent techniques. Dr. Ahn presented data from his center's registry, demonstrating that proximal Left Main stent area significantly impacts clinical outcomes. Larger minimum stent areas correlated with favorable long-term outcomes, challenging the conventional belief that simple crossover stenting inherently results in lower event rates.
Addressing this gap, Dr. Ahn presented new MSA criteria based on a study of 292 patients with unprotected LMCAD treated with the crush technique. This study focused on major adverse cardiovascular events (MACE), a composite of death, myocardial infarction, or repeat revascularization. Dr. Ahn's analysis revealed a linear relationship between MSA of LAD and LCX with MACEs. Larger IVUS-MSAs were associated with improved clinical outcomes, underlining the significance of this parameter in guiding interventions.
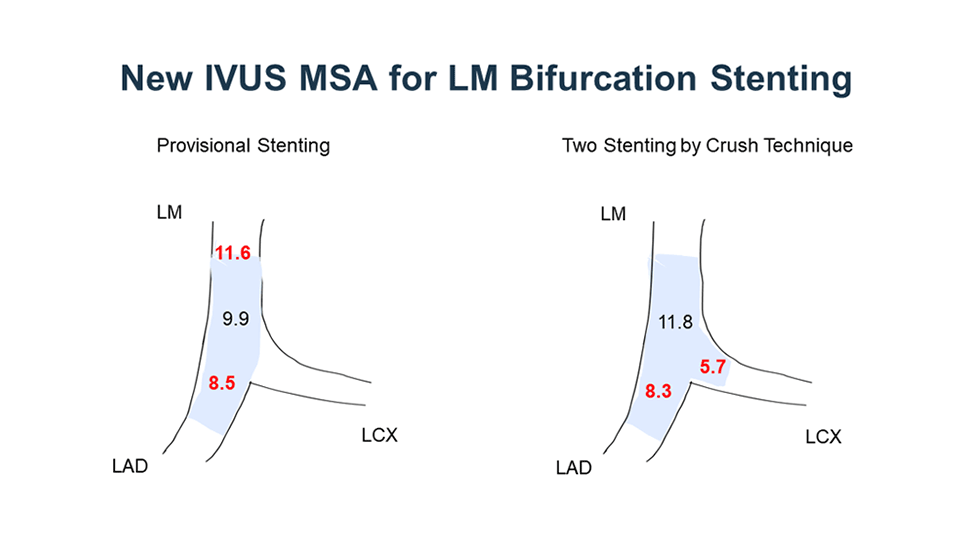
Dr. Ahn concluded his presentation by recommending optimal IVUS-MSA criteria for predicting 5-year MACE: 11.8 mm2 for the distal LM, 8.3 mm2 for the LAD ostium, and 5.7 mm2 for the LCX ostium. His findings stress the paramount importance of achieving an adequately large MSA under IVUS guidance during LM two-stenting procedures to mitigate adverse clinical events. These conclusions offer invaluable guidance for interventionists, enhancing the precision and effectiveness of treatment for patients undergoing LM two-stenting procedures.
Edited by

Ju Hyeon Kim, MD
Korea University Anam Hospital, Korea (Republic of)

KyungAe Kim, RN
CardioVascular Research Foundation (CVRF), Korea (Republic of)

Jung-Min Ahn
Asan Medical Center, Republic of Korea
Dr. Jung-Min Ahn of Asan Medical Center, Korea, delivered an enlightening study on Left Main (LM) percutaneous coronary intervention (PCI), focusing on optimizing two-stent techniques for LM bifurcation stenting, especially in the Left Anterior Descending (LAD) and Left Circumflex (LCX) arteries.
Delving into the challenge of determining significant LM disease, Dr. Ahn highlighted the difficulty in measuring fractional flow reserve (FFR), particularly in cases involving distal downstream disease. His research demonstrated a significant correlation between the minimum lumen area (MLA) in the LM and FFR values. An MLA less than 4.5 showed a high positive predictive value for FFR values less than 80, providing a potential criterion for identifying functionally significant disease.
Dr. Ahn's research contributes significantly to the field, considering the default strategy for treating bifurcation lesions in Left Main Coronary Artery Disease (LMCAD) has been a simple crossover from the LM to the LAD artery. However, instances where two-stenting cannot be avoided were noted. The ongoing debate on provisional versus two-stent techniques, as seen in trials like DK-CRUSH V and EBC-MAIN, emphasized the need for clearer criteria, especially as a substantial proportion of patients initially categorized for provisional stenting end up receiving two stents.
The necessity for this approach is evident from various trials on LMCAD, including PRECOMBAT, EXCEL, and NOBLE, where a significant proportion of patients received two-stent techniques. Even in the EBC-MAIN trial, which generally favored one stenting, about 22% of patients in the provisional stenting group ended up receiving two stents, underscoring the importance of understanding how to optimize the two-stent technique for better clinical outcomes.
Addressing the ambiguity in defining when to choose between the two techniques, Dr. Ahn discussed the current lack of definitive criteria. While angiographic criteria have been suggested, the absence of Intravascular Ultrasound (IVUS) criteria remains a gap. He proposed integrating IVUS criteria into decision-making processes, referencing studies indicating the predictive value of minimal lumen area and plaque burden for functional outcomes.
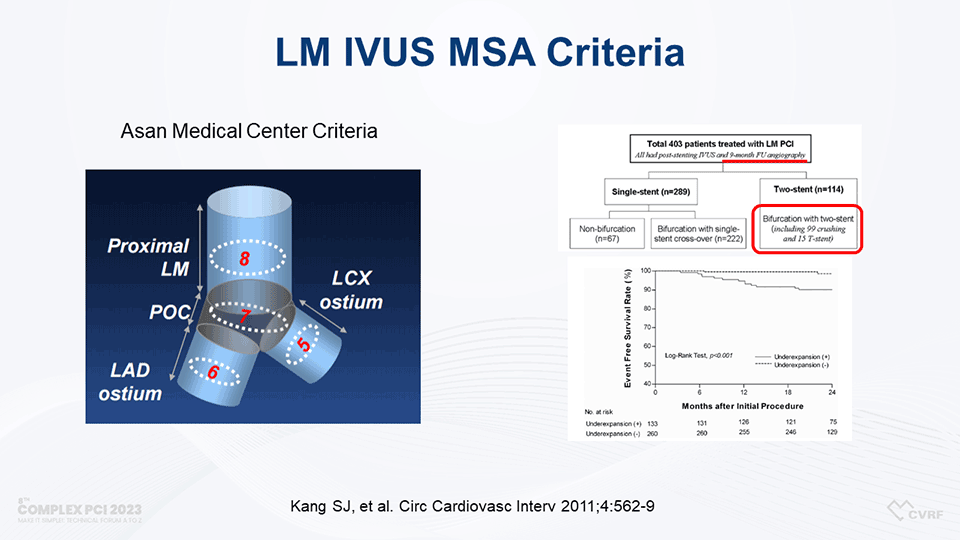
Dr. Ahn revisited the criteria established by Kang in 2011 while exploring the optimization of two-stent techniques. Kang et al. (2011) reported on minimal stent area (MSA) criteria for LM intravascular ultrasound (IVUS) from a diverse group of 403 patients undergoing LM PCI. However, the study's heterogeneity called for more specific MSA criteria, particularly concerning the LM crush technique. It's noteworthy that the EXCEL trial suggested a larger MSA compared to the established LM IVUS MSA criteria.
Emphasizing the necessity of refining these criteria, especially considering the heterogeneity of various stenting techniques, Dr. Ahn's recent analysis indicated that achieving larger minimum stent areas, particularly in the complex ostium of the Left Main, correlates with improved long-term outcomes. These findings offer potential benchmarks for optimizing stent size and contribute to the ongoing discussion on refining criteria for LM PCI.
The lecture provided insights into the ongoing debate about event rates between simple crossover and two-stent techniques. Dr. Ahn presented data from his center's registry, demonstrating that proximal Left Main stent area significantly impacts clinical outcomes. Larger minimum stent areas correlated with favorable long-term outcomes, challenging the conventional belief that simple crossover stenting inherently results in lower event rates.
Addressing this gap, Dr. Ahn presented new MSA criteria based on a study of 292 patients with unprotected LMCAD treated with the crush technique. This study focused on major adverse cardiovascular events (MACE), a composite of death, myocardial infarction, or repeat revascularization. Dr. Ahn's analysis revealed a linear relationship between MSA of LAD and LCX with MACEs. Larger IVUS-MSAs were associated with improved clinical outcomes, underlining the significance of this parameter in guiding interventions.
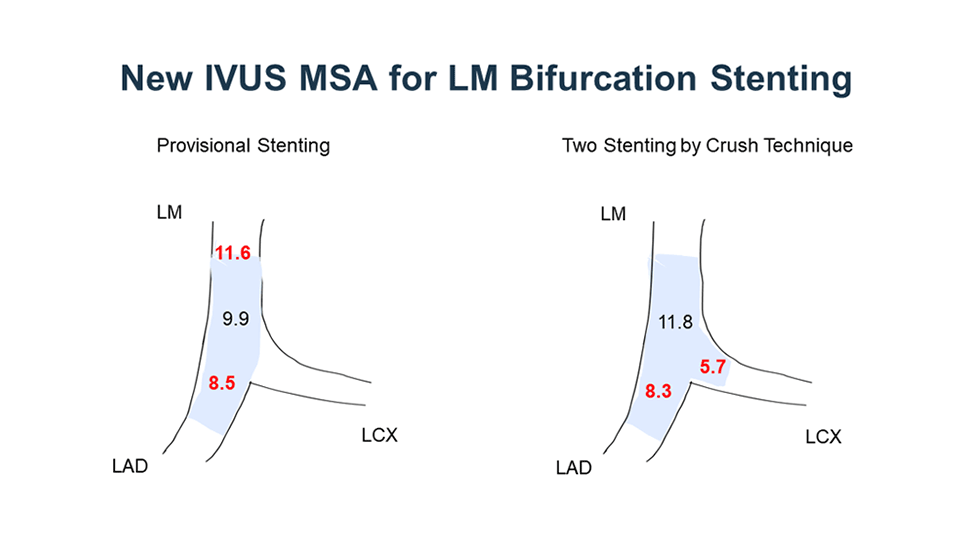
Dr. Ahn concluded his presentation by recommending optimal IVUS-MSA criteria for predicting 5-year MACE: 11.8 mm2 for the distal LM, 8.3 mm2 for the LAD ostium, and 5.7 mm2 for the LCX ostium. His findings stress the paramount importance of achieving an adequately large MSA under IVUS guidance during LM two-stenting procedures to mitigate adverse clinical events. These conclusions offer invaluable guidance for interventionists, enhancing the precision and effectiveness of treatment for patients undergoing LM two-stenting procedures.
Edited by

Ju Hyeon Kim, MD
Korea University Anam Hospital, Korea (Republic of)

KyungAe Kim, RN
CardioVascular Research Foundation (CVRF), Korea (Republic of)

Leave a comment