News | SummitMD
POST-PCI raises red flags for routine functional testing in high-risk PCI patients
2-year follow-up of PCI patients at high anatomical, clinical risk showed no survival benefits with surveillance testing over standard care
 Routine functional testing did not outperform standard care for major outcomes, including survival at 2-years, in high-risk patients undergoing percutaneous coronary intervention (PCI), a randomized study recently showed.
Routine functional testing did not outperform standard care for major outcomes, including survival at 2-years, in high-risk patients undergoing percutaneous coronary intervention (PCI), a randomized study recently showed.
The “Pragmatic trial comparing symptom-Oriented versus routine Stress Testing in high-risk patients undergoing Percutaneous Coronary Intervention” (POST-PCI) trial found no significant difference between the two follow-up strategies for the composite primary outcome of all-cause mortality, myocardial infarction (MI) and hospitalization for unstable angina (5.5% vs. 6.0%; HR 0.90, 95% CI, 0.61-1.35; p=0.62).
Principal investigator Duk-woo Park, MD, PhD (Asan Medical Center, Seoul, South Korea) presented the results at the European Society of Cardiology (ESC) Congress 2022 in Barcelona, Spain on Aug 28 with results published simultaneously in the New England Journal of Medicine (NEJM).
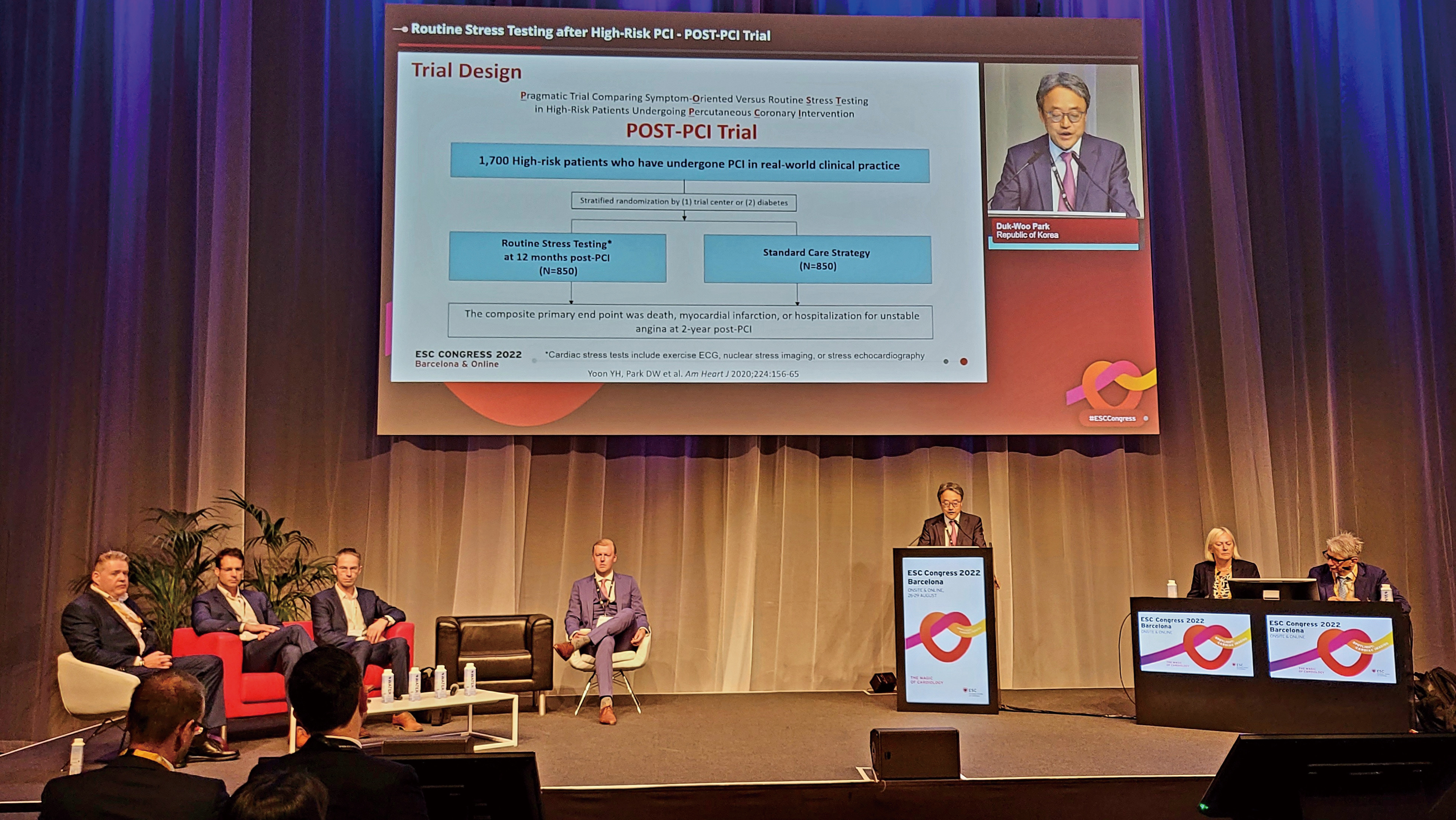
Duk-woo Park, MD, PhD (Asan Medical Center, Seoul, South Korea) presents POST-PCI findings at the ESC Congress 2022 held in Barcelona, Spain on Aug 28.
“There were no significant between-group differences for the primary composite of death, MI or hospitalization for unstable angina at 2-years between PCI and standard care,” Park said at the late-breaking science session. “The incidence of events was lower than expected in the two investigational groups, possibly due to improved techniques for complex PCI along with general improvements in cardiovascular care over the years.”
“Nevertheless, routine stress testing was associated with more invasive coronary angiography and repeat revascularization after 1-year without a significant reduction in major cardiovascular events or mortality,” he said. “Our trial does not support active surveillance with routine functional testing as a follow-up strategy in high-risk patients undergoing PCI.”
POST-PCI
The multicenter, pragmatic, randomized superiority trial included high-risk patients undergoing PCI at 11 centers in South Korea to evaluate whether routine stress testing would significantly reduce ischemic cardiovascular events or mortality over standard care.
Our trial does not support active surveillance with routine functional testing as a follow-up strategy in high-risk patients who undergo PCI.
Also examined was whether routine functional testing changed post-PCI management practice or other preventive strategies, including preemptive angiography, revascularization and more aggressive medical therapies.
Investigators enrolled 1,700 patients (mean age: 65 years; 80% male) and randomized them by trial center or diabetes status to post-PCI management with routine stress testing at 1-year after PCI (n=850) or standard care (n=850).
Patients’ high-risk anatomical characteristics included left main (LM) disease (21.0%), bifurcation lesions (43.5%), multivessel disease (69.8%) and diffuse long lesions (70.1%). High-risk clinical characteristics included medically-treated diabetes (38.7%) and prior treatment with DES (96.4%).
Other high-risk factors included restenosis, bypass graft disease, chronic renal failure and enzyme-positive acute coronary syndrome (ACS).
All patients underwent successful PCI with contemporary drug-eluting stents, bioresorbable scaffolds or drug-coated balloons. Cardiac stress testing included exercise echocardiography (ECG), nuclear stress imaging or stress ECG.
The composite primary endpoint was defined as death, MI or hospitalization for unstable angina 2-years after randomization. Secondary endpoints included individual components of the primary composite outcome, composite of death or MI, all-cause hospitalization, invasive coronary angiography and repeat revascularization procedures.
Results showed that routine functional testing had a statistically non-significant trend for the primary outcomes compared to standard care (5.5% vs. 6.0%; HR 0.90, 95% CI, 0.61-1.35; p=0.62).
We must refrain from prescribing surveil¬lance stress testing after PCI in the absence of other clinical signs or symptoms suggestive of stent failure.
For secondary outcomes, there were no significant differences for the individual components of all-cause mortality (routine testing 2.8% vs. standard care 3.3%; HR 0.82, 0.48-1.43), MI (0.5% vs. 1.2%; HR 0.40, 0.13-1.28) and hospitalization for unstable angina (2.3% vs. 1.7%; HR 1.36, 0.68-2.72).
Outcomes for invasive cardiac catheterization (11.9% vs. 9.0%; log-rank P=0.07) and repeat revascularization (7.8% vs. 5.6%; log-rank P=0.09) also showed no significant improvements with functional stress testing.
Furthermore, landmark analysis performed at 1-year and 2-years after PCI showed functional testing was associated with a 2-fold higher incidence of invasive coronary angiography that did not lead to meaningful reductions in all-cause mortality or MI rates.
On study limitations, Park cited the possibility of ascertainment bias due to unmasked follow-up strategies (from patients and investigators); varying diagnostic accuracy of the stress tests; cases of nonadherence to stress testing; and no analysis of quality of life, cost-effectiveness or radiation exposure.
‘Compelling’ evidence nudges ‘post’-surveillance testing era, guideline changes?
The new evidence could spark changes in coronary artery guidelines, an expert commented, shifting the existing weak recommendations on surveillance testing to a Class III recommendation for high-risk patients, indicating contraindication.
“The POST-PCI trial provides compelling new evidence for a future class III recommendation for routine surveillance testing after PCI,” wrote Jacqueline E. Tamis‑Holland, MD (Mount Sinai Morningside Hospital, New York, USA) in a NEJM editorial published Aug 28. “Until then, we must refrain from prescribing surveil¬lance stress testing to our patients after PCI, in the absence of other clinical signs or symptoms suggestive of stent failure.”
Currently, the 2021 American College of Cardiology, American Heart Association and Society of Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines have no recommendations on routine stress testing after revascularization, citing limited RCT data on the subject.
The 2018 European Society of Cardiology and European Association for Cardio-Thoracic Surgery (ESC/EACTS) guidelines gave a weak Class IIb recommendation (level of evidence C) for surveillance with non-invasive imaging-based stress testing in high-risk patients 6-months after revascularization.
European guidelines also gave the Class IIb recommendation (level of evidence C) for late surveillance angiography (3-12 months after PCI) in high-risk patients (i.e., unprotected LM stenosis) and routine non-invasive imaging-based stress testing 1 year after PCI or 5 years after coronary artery bypass graft (CABG).
POST-PCI provides compelling new evidence for a future class III recommendation for routine surveillance testing after PCI.
Despite weak guideline recommendations on surveillance testing, real-world observational studies have reported their widespread use in patients after CABG and PCI, with more than half of patients reported to have undergone functional testing within 2 years of coronary revascularization.
“Studies have demonstrated a substantially high rate of repeat revascularization in hospitals that had the highest frequency of stress testing after PCI, and this did not translate to lower risk of MI or death during long-term follow-up,” Tamis-Holland wrote.
Tamis-Holland noted that POST-PCI results also back findings from ISCHEMIA - the landmark, randomized trial on high-risk, moderate-to-severe ischemic patients on stress testing that reported no substantial difference between an initial invasive strategy and conservative treatment. In ISCHEMIA, around 20% had previously undergone PCI and roughly one-third had symptoms of angina 4 weeks before randomization.
“Despite the inclusion of only high-risk patients [in ISCHEMIA], there was no substantial difference between the two strategies in the primary clinical endpoint at 5 years of follow-up,” she observed. “The extent of ischemia on stress testing did not identify a subgroup of patients that derived a benefit from an invasive strategy.”
“Collectively, the trials highlight the lack of benefit with rou¬tine stress testing in asymptomatic patients, underscoring the importance of proper procedural techniques and aggressive secondary prevention to improve outcomes after PCI.”
Edited by

Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
Taeoh Kim, MD
Asan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read Biography
Park, Duk-Woo, et al. “Routine Functional Testing or Standard Care in High-Risk Patients after PCI.” New England Journal of Medicine, vol. 387, no. 10, 2022, pp. 905–915., doi:10.1056/nejmoa2208335.
Tamis-Holland, Jacqueline E. “Surveillance Stress Testing ‘POST-PCI’ — a Future Class III Recommendation?” New England Journal of Medicine, vol. 387, no. 10, 2022, pp. 941–942., doi:10.1056/nejme2210021.
POST-PCI was supported by an investigator-initiated grant from the CardioVascular Research Foundation (Seoul, South Korea) and Daewoong Pharmaceutical.
 Routine functional testing did not outperform standard care for major outcomes, including survival at 2-years, in high-risk patients undergoing percutaneous coronary intervention (PCI), a randomized study recently showed.
Routine functional testing did not outperform standard care for major outcomes, including survival at 2-years, in high-risk patients undergoing percutaneous coronary intervention (PCI), a randomized study recently showed.
The “Pragmatic trial comparing symptom-Oriented versus routine Stress Testing in high-risk patients undergoing Percutaneous Coronary Intervention” (POST-PCI) trial found no significant difference between the two follow-up strategies for the composite primary outcome of all-cause mortality, myocardial infarction (MI) and hospitalization for unstable angina (5.5% vs. 6.0%; HR 0.90, 95% CI, 0.61-1.35; p=0.62).
Principal investigator Duk-woo Park, MD, PhD (Asan Medical Center, Seoul, South Korea) presented the results at the European Society of Cardiology (ESC) Congress 2022 in Barcelona, Spain on Aug 28 with results published simultaneously in the New England Journal of Medicine (NEJM).
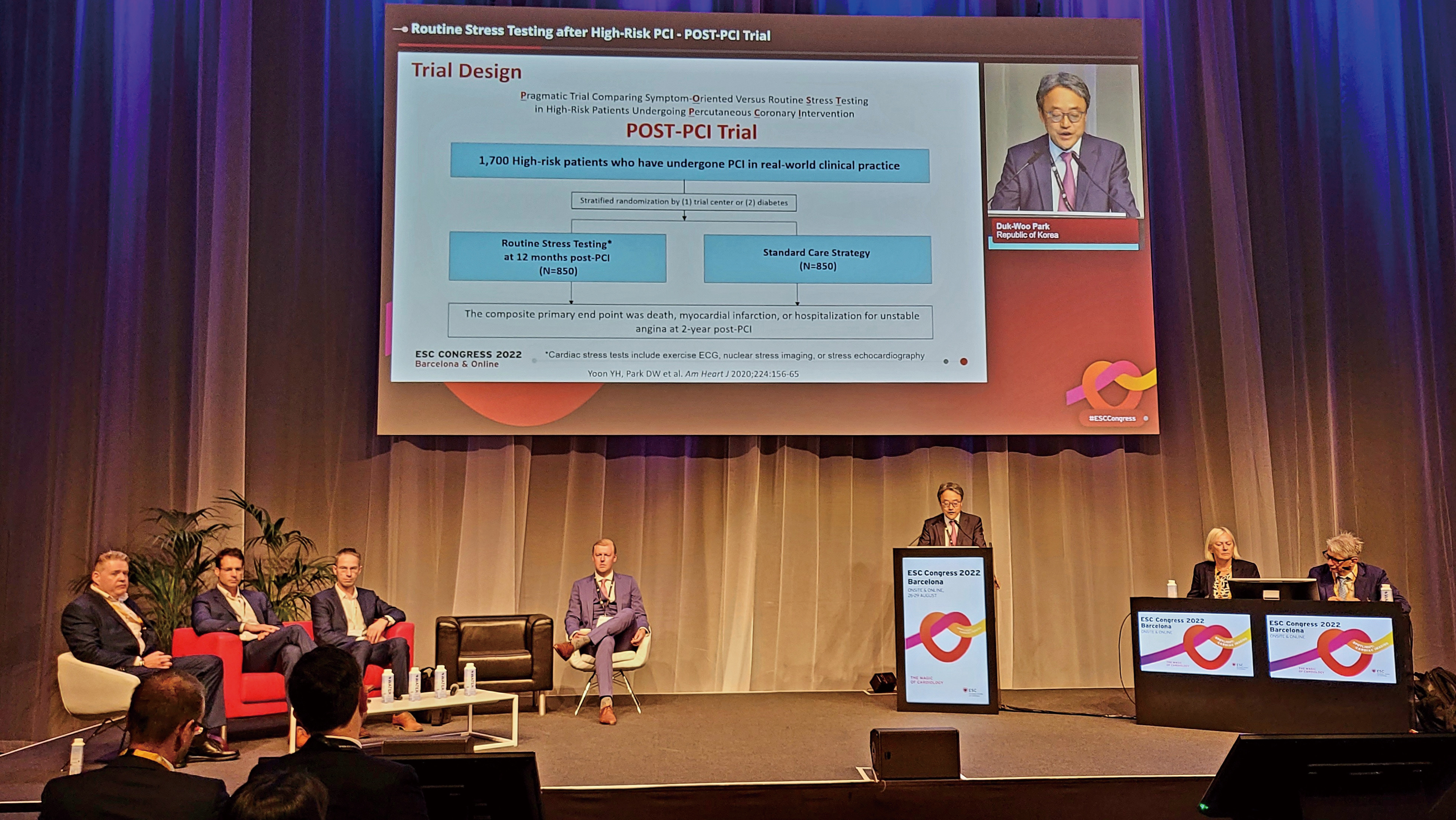
Duk-woo Park, MD, PhD (Asan Medical Center, Seoul, South Korea) presents POST-PCI findings at the ESC Congress 2022 held in Barcelona, Spain on Aug 28.
“There were no significant between-group differences for the primary composite of death, MI or hospitalization for unstable angina at 2-years between PCI and standard care,” Park said at the late-breaking science session. “The incidence of events was lower than expected in the two investigational groups, possibly due to improved techniques for complex PCI along with general improvements in cardiovascular care over the years.”
“Nevertheless, routine stress testing was associated with more invasive coronary angiography and repeat revascularization after 1-year without a significant reduction in major cardiovascular events or mortality,” he said. “Our trial does not support active surveillance with routine functional testing as a follow-up strategy in high-risk patients undergoing PCI.”
POST-PCI
The multicenter, pragmatic, randomized superiority trial included high-risk patients undergoing PCI at 11 centers in South Korea to evaluate whether routine stress testing would significantly reduce ischemic cardiovascular events or mortality over standard care.
Our trial does not support active surveillance with routine functional testing as a follow-up strategy in high-risk patients who undergo PCI.
Also examined was whether routine functional testing changed post-PCI management practice or other preventive strategies, including preemptive angiography, revascularization and more aggressive medical therapies.
Investigators enrolled 1,700 patients (mean age: 65 years; 80% male) and randomized them by trial center or diabetes status to post-PCI management with routine stress testing at 1-year after PCI (n=850) or standard care (n=850).
Patients’ high-risk anatomical characteristics included left main (LM) disease (21.0%), bifurcation lesions (43.5%), multivessel disease (69.8%) and diffuse long lesions (70.1%). High-risk clinical characteristics included medically-treated diabetes (38.7%) and prior treatment with DES (96.4%).
Other high-risk factors included restenosis, bypass graft disease, chronic renal failure and enzyme-positive acute coronary syndrome (ACS).
All patients underwent successful PCI with contemporary drug-eluting stents, bioresorbable scaffolds or drug-coated balloons. Cardiac stress testing included exercise echocardiography (ECG), nuclear stress imaging or stress ECG.
The composite primary endpoint was defined as death, MI or hospitalization for unstable angina 2-years after randomization. Secondary endpoints included individual components of the primary composite outcome, composite of death or MI, all-cause hospitalization, invasive coronary angiography and repeat revascularization procedures.
Results showed that routine functional testing had a statistically non-significant trend for the primary outcomes compared to standard care (5.5% vs. 6.0%; HR 0.90, 95% CI, 0.61-1.35; p=0.62).
We must refrain from prescribing surveil¬lance stress testing after PCI in the absence of other clinical signs or symptoms suggestive of stent failure.
For secondary outcomes, there were no significant differences for the individual components of all-cause mortality (routine testing 2.8% vs. standard care 3.3%; HR 0.82, 0.48-1.43), MI (0.5% vs. 1.2%; HR 0.40, 0.13-1.28) and hospitalization for unstable angina (2.3% vs. 1.7%; HR 1.36, 0.68-2.72).
Outcomes for invasive cardiac catheterization (11.9% vs. 9.0%; log-rank P=0.07) and repeat revascularization (7.8% vs. 5.6%; log-rank P=0.09) also showed no significant improvements with functional stress testing.
Furthermore, landmark analysis performed at 1-year and 2-years after PCI showed functional testing was associated with a 2-fold higher incidence of invasive coronary angiography that did not lead to meaningful reductions in all-cause mortality or MI rates.
On study limitations, Park cited the possibility of ascertainment bias due to unmasked follow-up strategies (from patients and investigators); varying diagnostic accuracy of the stress tests; cases of nonadherence to stress testing; and no analysis of quality of life, cost-effectiveness or radiation exposure.
‘Compelling’ evidence nudges ‘post’-surveillance testing era, guideline changes?
The new evidence could spark changes in coronary artery guidelines, an expert commented, shifting the existing weak recommendations on surveillance testing to a Class III recommendation for high-risk patients, indicating contraindication.
“The POST-PCI trial provides compelling new evidence for a future class III recommendation for routine surveillance testing after PCI,” wrote Jacqueline E. Tamis‑Holland, MD (Mount Sinai Morningside Hospital, New York, USA) in a NEJM editorial published Aug 28. “Until then, we must refrain from prescribing surveil¬lance stress testing to our patients after PCI, in the absence of other clinical signs or symptoms suggestive of stent failure.”
Currently, the 2021 American College of Cardiology, American Heart Association and Society of Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines have no recommendations on routine stress testing after revascularization, citing limited RCT data on the subject.
The 2018 European Society of Cardiology and European Association for Cardio-Thoracic Surgery (ESC/EACTS) guidelines gave a weak Class IIb recommendation (level of evidence C) for surveillance with non-invasive imaging-based stress testing in high-risk patients 6-months after revascularization.
European guidelines also gave the Class IIb recommendation (level of evidence C) for late surveillance angiography (3-12 months after PCI) in high-risk patients (i.e., unprotected LM stenosis) and routine non-invasive imaging-based stress testing 1 year after PCI or 5 years after coronary artery bypass graft (CABG).
POST-PCI provides compelling new evidence for a future class III recommendation for routine surveillance testing after PCI.
Despite weak guideline recommendations on surveillance testing, real-world observational studies have reported their widespread use in patients after CABG and PCI, with more than half of patients reported to have undergone functional testing within 2 years of coronary revascularization.
“Studies have demonstrated a substantially high rate of repeat revascularization in hospitals that had the highest frequency of stress testing after PCI, and this did not translate to lower risk of MI or death during long-term follow-up,” Tamis-Holland wrote.
Tamis-Holland noted that POST-PCI results also back findings from ISCHEMIA - the landmark, randomized trial on high-risk, moderate-to-severe ischemic patients on stress testing that reported no substantial difference between an initial invasive strategy and conservative treatment. In ISCHEMIA, around 20% had previously undergone PCI and roughly one-third had symptoms of angina 4 weeks before randomization.
“Despite the inclusion of only high-risk patients [in ISCHEMIA], there was no substantial difference between the two strategies in the primary clinical endpoint at 5 years of follow-up,” she observed. “The extent of ischemia on stress testing did not identify a subgroup of patients that derived a benefit from an invasive strategy.”
“Collectively, the trials highlight the lack of benefit with rou¬tine stress testing in asymptomatic patients, underscoring the importance of proper procedural techniques and aggressive secondary prevention to improve outcomes after PCI.”
Edited by

Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
Taeoh Kim, MD
Asan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read BiographyPark, Duk-Woo, et al. “Routine Functional Testing or Standard Care in High-Risk Patients after PCI.” New England Journal of Medicine, vol. 387, no. 10, 2022, pp. 905–915., doi:10.1056/nejmoa2208335.
Tamis-Holland, Jacqueline E. “Surveillance Stress Testing ‘POST-PCI’ — a Future Class III Recommendation?” New England Journal of Medicine, vol. 387, no. 10, 2022, pp. 941–942., doi:10.1056/nejme2210021.

Leave a comment