COMPLEX PCI 2022
Guideline and concept changes: revascularization for Left Main in 2022
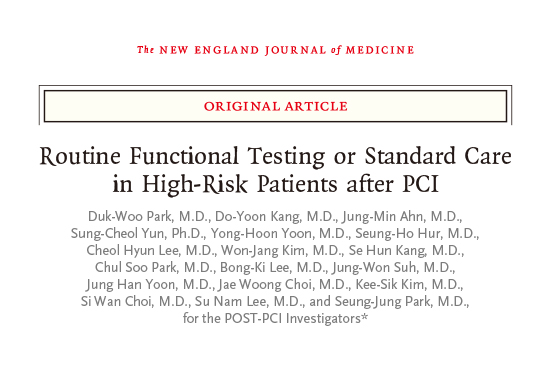
Percutaneous coronary intervention (PCI) may not lower mortality risk more than bypass surgery in left main (LM) – a leading interventional cardiologist said – but both are complementary strategies for achieving different clinical endpoints, making patient preference important. “Evidence generated so far makes it safe to say that PCI does not improve survival more than coronary artery bypass grafting (CABG) in patients with stable ischemic heart disease (SIHD),” Duk-Woo Park, MD, PhD (Asan Medical Center, Korea), said at COMPLEX PCI 2022 on Nov 24 at the Grand Walkerhill Seoul in South Korea. He presents evolving concepts and guideline recommendations on revascularization for LM disease at the COMPLEX PCI 2022 conference held at the Grand Walkerhill Seoul in South Korea on Nov 24. “However, PCI plays a key role in acute coronary syndrome (ACS), especially for improving patient-oriented outcomes of angina patients who are either unresponsive to medical therapy, unwilling to take anti-anginal medication or unwilling to undergo invasive CABG,” he said. Although tradition held CABG as the gold standard of treatment for a wide spectrum of SIHD patients, especially those with LM-coronary artery disease (CAD), technological and technical advancements in PCI and optimal medical therapy (OMT) spurred requests to replace “outdated” studies that cast PCI in an unfavorable light against OMT and CABG. As an interventional cardiologist, the evidence generated so far makes it safe to say that PCI does not improve survival more than CABG in SIHD. Both older and more recent studies on SIHD – including MASS II (2004), COURAGE (2007), BARI 2D (2009) and FAME-2 (2012) – had shown negative or neutral results with PCI compared to OMT for the “hard” clinical endpoints of all-cause or cardiovascular (CVD) mortality. Studies on multivessel disease (MVD) – including the SYNTAX (2019), BEST (2015), FREEDOM (2012) and FAME-3 (2022) trials – also found lower rates of major adverse cardiovascular events (MACE) with CABG compared to PCI. However, contemporary studies incorporating state-of-the-art PCI – including SYNTAX-LM (2010), PRECOMBAT (2011) and EXCEL (2016) – began demonstrating comparable outcomes between stenting and surgery, reporting no statistically significant difference between PCI and CABG for all-cause mortality and the primary endpoint. Studies on state-of-the-art PCI versus CABG in LM disease.Source: Dr. Park's slides at COMPLEX PCI 2022 Notably, the 10-year follow-up results for mortality from SYNTAX-LM(CABG 26.7% vs. PCI 26.1%; HR 0.90; 95% CI; 0.68-1.20; P=0.47) and AMC’s 10-year PRECOMBAT LM (CABG 13.8% vs. PCI 14.5%; HR 1.13; 95% CI; 0.75-1.70; P=0.57) further signaled comparability between strategies. The 5-year follow-up of the EXCEL trial, which reported comparable outcomes between bypass surgery and PCI for major adverse cardiac and cerebrovascular events (MACCE), infamously came under fire for controversial interpretations of outcomes and fueled the debate between cardiac surgeons and interventionalists. Along with significant study limitations of the EXCEL trial – including underpowered outcomes (“prone to false negatives”), no adjustment for multiplicity (“prone to false positives”) and no P-values (“not designed for hypothesis testing”) –other contemporary studies, like the REVIVED-BCIS2 study also found no survival benefit with PCI over OMT, raising calls for more concrete data. PCI plays a key role in ACS by improving patient-oriented outcomes of angina patients who are either unresponsive to medical therapy, unwilling to take anti-anginal medication or unwilling to undergo invasive CABG. Interventional cardiologists tended to call for new randomized trials with “different patients, better stents, more IVUS or FFR, more follow-up or other trial endpoints” any time a new series of trials reported neutral or worse outcomes with PCI compared to OMT or CABG, he explained, despite the lack of mortality benefit with PCI: “The higher benefit of survival with CABG over PCI was a key issue in many (observational) studies like EXCEL and urged individual patient data (IPD) meta-analysis.” The highly anticipated meta-analysis – published in the Lancet last year by Marc S. Sabatine, MD (Brigham and Women's Hospital, Boston, USA) and investigators, including ones at AMC – found no significant difference in all-cause mortality between treatment arms (PCI 11.2% vs. CABG 10.2%; HR 1.10; 0.91-1.32; P=0.33), indicating a statistically non-significant absolute difference of 0.9% (-0.9-2.8). Outcomes of the meta-analysis, which encompassed the four major trials of SYNTAX Left Main, PRECOMBAT, NOBLE and EXCEL, also found no significant difference between PCI and CABG arms after adjusting for SYNTAX scores (HR 1.09; 0.91-1.31). Separate analysis of the SYNTAX and PRECOMBAT studies, both with follow-up to 10-years, demonstrated no significant between-group differences for the endpoint of all-cause mortality (CABG 22.1% vs. PCI 21.6%; HR 0.96; 0.76-1.21; P=0.72). The major finding, he said, was no difference for the primary outcome of all-cause mortality between PCI and CABG for LM patients at intermediate- or low-anatomic risk but each approach had tradeoffs: CABG with higher risks for stroke (CABG 3.1% vs. PCI 2.7%; HR 0.84; 0.59-1.21; P=0.36) and procedural MI (4.7% vs. 3.2%; HR 0.67; 0.48-0.93; P=0.015); PCI had higher rates of spontaneous MI (2.6% vs. 6.2%; HR 2.36; 1.71-3.23; P
December 15, 2022 8869