News | SummitMD
1-Month DAPT in High-Bleeding Risk Noninferior for Ischemic Outcomes, Less Bleeding: MASTER-DAPT
In HBR patients after DES-PCI, shorter 1-month DAPT showed noninferior NACE/MACCE rates with less major bleeds compared to 12-month DAPT
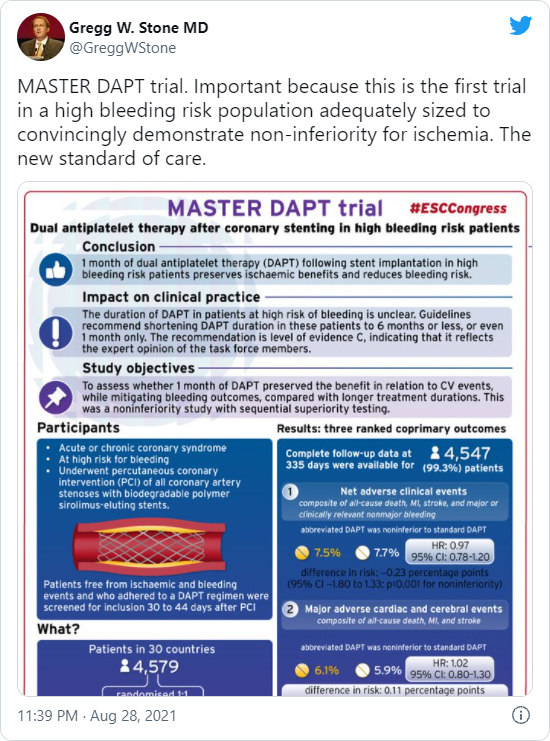
A shorter dual antiplatelet therapy (DAPT) of 1-month may become the "new standard of care" for a subgroup of coronary artery disease (CAD) patients after percutaneous coronary intervention (PCI), MASTER DAPT findings signaled.
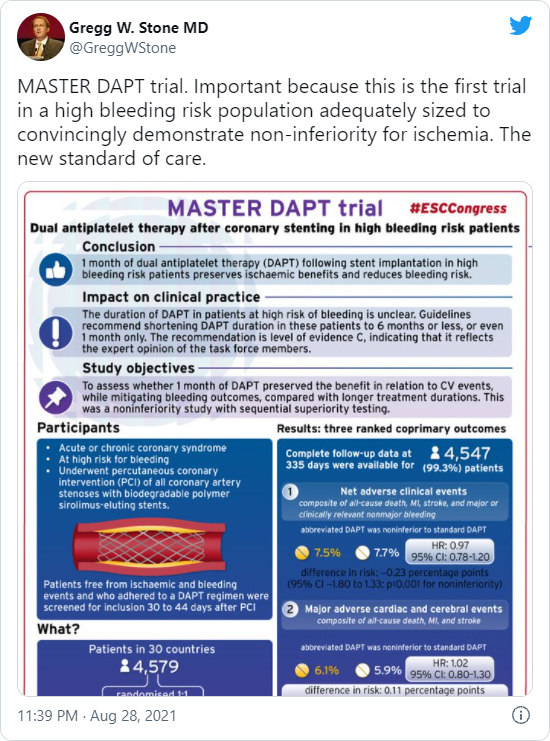
Results from the trial on high bleeding risk (HBR) patients showed that 1-month DAPT post-PCI was noninferior to a longer DAPT duration of at least 3 months for the primary outcomes of net adverse clinical events (NACE) and major adverse cardiac or cerebral events (MACCE) at 335 days.
The slashed DAPT duration also translated to lower incidence of major and clinically relevant nonmajor bleeding.
DAPT is a medication regimen that combines a P2Y12 receptor inhibitor (clopidogrel, ticagrelor, or prasugrel) and aspirin to reduce the risk of restenosis and prevent thrombotic complications.
Principal investigator Marco Valgimigli, MD (Cardiocentro Ticino Foundation, Lugano, Switzerland) presented the findings at a Hot Line session during the European Society of Cardiology (ESC) Congress 2021 on Aug. 28, with the paper published simultaneously in the New England Journal of Medicine (NEJM)1.
"1-month DAPT after PCI in HBR patients maintained the ischemic benefits of therapy while reducing bleeding risk," Valgimigli said. "These results can inform treatment decisions regarding DAPT in PCI-HBR patients, including those with clinical or angiographic high ischemic risk features who do not present postprocedural ischemic events."
Major guidelines have broadly endorsed a DAPT duration of at least 12 months after PCI as the standard. However, an evolving PCI landscape and continuing research on subgroups have highlighted that standard DAPT may not be optimal for all PCI patients.
Notably, the optimal DAPT duration for HBR patients has remained unclear. The advent of drug-eluting stents (DES) -particularly second-generation DES -and the entry of more potent P2Y12 inhibitors have confounded the problem.
In the increasingly complex HBR arena, clinicians have identified a trend of DAPT outcomes that varies on the duration of the regimen; namely, longer DAPT lowers ischemic risk at the expense of higher bleeding risk, while shorter DAPT reduces bleeding risk but elevates ischemic risk.
Swinging on this pendulum of elevated ischemic or bleeding risk, physicians have leaned on analyzing individual patient characteristics to strike the right balance between the risks and benefits of DAPT.
MASTER DAPT serves as the largest and "first important" randomized trial to report positive results for shorter DAPT in HBR patients, paving the way forward to a new standard of care, according to Gregg W. Stone, MD (Icahn School of Medicine at Mount Sinai, New York, USA).
MASTER DAPT: Key Takeaways
Investigator-initiated, multicenter, randomized, open-label, noninferiority trial
Conducted from February 2017 to December 2019 at 140 sites in 30 countries
- Patient enrollment/characteristics
- Enrollment: 4,579 HBR patients with acute/chronic coronary syndrome undergone successful PCI with biodegradable-polymer sirolimus-eluting stent (Ultimaster, Terumo) (mean age: 76 years; 69.3% men)
- Comorbidities: diabetes 33.6%, chronic kidney disease 18.9%, previous cerebrovascular event 12.4%, peripheral vascular disease 10.6%, concomitant oral anticoagulation 36.4%
- Study design
- 1:1 randomization after PCI (median time from index PCI to randomization: 34 days)
- Randomized to either abbreviated-DAPT (n=2,295) or standard-DAPT (n=2,284)
-
Follow-up data at 335 days for 4,547 patients
- Primary outcomes (abbreviated- vs. standard-DAPT)
- NACE: 7.5% vs. 7.7% (HR 0.97; 95% CI; 0.78-1.20)
(risk difference -0.23%p, 95% CI, -1.80 to 1.33; p<0.001 for noninferiority)
- MACCE: 6.1% vs. 5.9% (HR 1.02, 0.80-1.30)
(risk diff. 0.11%p; -1.29 to 1.51; p=0.001 for noninferiority)
- Major/clinically relevant nonmajor bleeding: 6.5% vs. 9.4% (HR 0.68, 0.55-0.84)
(risk diff. -2.82%p, -4.40 to -1.24; p<0.001 for superiority)
- Secondary outcomes (abbreviated- vs. standard-DAPT)
- All-cause mortality: 3.3% vs. 3.6% (HR 0.92, 0.67-1.26)
- Myocardial infarction (MI): 2.7% vs. 2.2% (HR 1.22, 0.84-1.78)
- Definite/probable stent thrombosis: 0.6% vs. 0.4% (HR 1.55, 0.67-3.57)
- Cerebrovascular events: 0.8% vs. 1.4% (HR 0.53, 0.29-0.95)
- Stroke: 0.5% vs. 1.0% (HR 0.52, 0.26-1.04)
- BARC type 2 bleeding: 4.5% vs. 6.8% (diff. -2.25%p, -3.59 to -0.90)
- bleeding type 3, 4, 5: 2.3% vs. 2.6%
- BARC type 5 bleeding (fatal): 0.1% vs. 0.4%
Valgimigli stressed that the trial "did not exclude patients with ACS or limit the number, location, or complexity of the treated lesions, unlike other studies" - raising hopes for short DAPT in HBR to maintain ischemic benefits without increasing the risk of adverse clinical events of MI, stroke, major bleeding, and death.
1-month DAPT 'masters' 3 primary outcomes
Although previous studies, such as GLOBAL LEADERS, STOPDAPT-2, ISAR-TRIPLE, DAPT, and PEGASUS-TIMI-54, had examined the safety and efficacy of shorter DAPT, many fell short in suggesting the optimal regimen duration in HBR.
Limitations in study design (i.e., nonrandomization) or strict enrollment criteria such as excluding ACS or complex PCI patients produced inconsistent results that varied according to population characteristics.
Unlike other studies, MASTER DAPT didn’t exclude patients with ACS or limit the number, location, or complexity of treated lesions.
Clinicians have since tailored DAPT duration to the individual patient, while calling for randomized trials that illuminate optimal DAPT for HBR patients.
The investigator-initiated, multicenter, randomized, open-label MASTER DAPT trial honed in on the HBR subgroup and tested the noninferiority of abbreviated-DAPT against standard DAPT in 4,579 patients.
Protocol called for patients in the short-DAPT arm to immediately discontinue DAPT after randomization and continue with single antiplatelet therapy (SAPT) until trial completion. The standard-DAPT arm continued DAPT for 5 additional months (6 months post-PCI) and then continued to antiplatelet monotherapy.
Exceptions were made for patients indicated for oral anticoagulation (OAC). Those on OAC in the short DAPT arm continued SAPT for up to 6 months after PCI. OAC takers in the standard arm continued DAPT for at least 2 additional months (3 months post-PCI).
SAPT consisted of aspirin or a P2Y12 inhibitor, authors noted. Clopidogrel was the most frequently used P2Y12 inhibitor in the standard DAPT group and the most commonly used monotherapy in the abbreviated DAPT group.
The 3 ranked primary outcomes were NACE (composite of death from any cause, MI, stroke, or major bleeding), MACCE (composite of death from any cause, MI or stroke), and major bleeding (BARC type 3, 5) as well as major or clinically relevant nonmajor bleeding (BARC type 2, 3, 5).
Results showed that shorter DAPT, lasting a median of 34 days after PCI, and standard DAPT over a median of 193 days post-PCI showed similar rates of NACE and MACCE.
Shorter DAPT was also superior for major bleeding or clinically relevant nonmajor bleeding outcomes.
Subgroup analysis of MASTER DAPT published in Circulation2 on Aug. 29 on 36% of HBR-PCI patients on OAC versus those not on OAC showed shortening DAPT did not increase ischemic events in patients regardless of OAC administration.
The analysis also showed that BARC 2, 3, or 5 bleeding did not differ significantly with OAC indication, but bleeding rates were lower in the abbreviated DAPT arm not indicated for OAC.
Findings from MASTER-DAPT can be applied directly to a contemporary, real-world setting that includes a diverse group of HBR patients that require DAPT after ACS/PCI
These findings - in line with current recommendations from the 2017 ESC/EACTS guideline and the 2020 ESC guideline for management of ACS in patients without ST-segment elevation for 1- to 6-month DAPT for HBR patients - are expected to ramp up the weak strength of the endorsement (LoE: C) that currently only reflects the opinion for task force members.
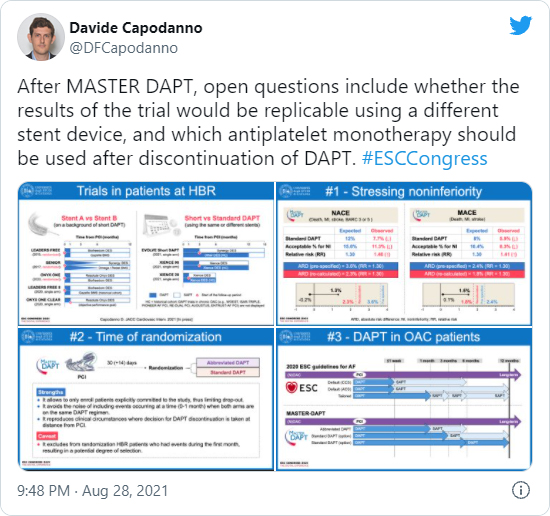
Pursuing discussion at ESC 2021and on Twitter asked whether the "game-changing" results could be applied to different stent devices and questioned the choice of SAPT after discontinuing DAPT.
In an accompanying editorial3, Erik Magnus Ohman, MD (Duke University School of Medicine, North Carolina, USA) welcomed the important findings for HBR patients that represent a “major shift” that “moves toward a shorter and simpler antithrombotic strategy after PCI, with concomitant shorter antiplatelet monotherapy for chronic disease after DES implantation.”
However, Ohman also cautioned that the use of abbreviated DAPT may be reasonable only in the context of the Ultimaster DES stent used in the trial, and may not be applicable to later-generation DES.
The noninferiority design also represents some challenges in interpreting study findings and determining an acceptable trade-off that supports shorter DAPT. For instance, although composite ischemic outcome showed noninferiority, the wide 95% CI for HR encompassed a potential 30% higher incidence in the short DAPT arm, which is “higher than some would consider to be a reasonable trade-off between bleeding and ischemic events.”
The wide confidence interval in MASTER DAPT, Ohman added, pales to the “tighter and relative” boundaries for noninferiority in previous trials, thereby calling for additional trials to replicate findings.
Until further trials help clear ambiguity from the HBR realm, many emphasized the wide applicability of MASTER-DAPT findings.
Duk-Woo Park, MD (Asan Medical Center, Seoul, South Korea) summarized findings and commented to SummitMD that: “The MASTER-DAPT trial demonstrated abbreviated 1-month DAPT may be optimal for safety and efficacy for HBR patients who had undergone implantation with a biodegradable polymer sirolimus-eluting stent for ACS for NACE, MACCE, and bleeding endpoints compared to 3-month DAPT. Findings from this trial can be directly applied to contemporary, real-world clinical practice, which is known for having a wide range of HBR patients who require DAPT after ACS or PCI.”
Edited by

Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read Biography
A shorter dual antiplatelet therapy (DAPT) of 1-month may become the "new standard of care" for a subgroup of coronary artery disease (CAD) patients after percutaneous coronary intervention (PCI), MASTER DAPT findings signaled.
Results from the trial on high bleeding risk (HBR) patients showed that 1-month DAPT post-PCI was noninferior to a longer DAPT duration of at least 3 months for the primary outcomes of net adverse clinical events (NACE) and major adverse cardiac or cerebral events (MACCE) at 335 days.
The slashed DAPT duration also translated to lower incidence of major and clinically relevant nonmajor bleeding.
DAPT is a medication regimen that combines a P2Y12 receptor inhibitor (clopidogrel, ticagrelor, or prasugrel) and aspirin to reduce the risk of restenosis and prevent thrombotic complications.
Principal investigator Marco Valgimigli, MD (Cardiocentro Ticino Foundation, Lugano, Switzerland) presented the findings at a Hot Line session during the European Society of Cardiology (ESC) Congress 2021 on Aug. 28, with the paper published simultaneously in the New England Journal of Medicine (NEJM)1.
"1-month DAPT after PCI in HBR patients maintained the ischemic benefits of therapy while reducing bleeding risk," Valgimigli said. "These results can inform treatment decisions regarding DAPT in PCI-HBR patients, including those with clinical or angiographic high ischemic risk features who do not present postprocedural ischemic events."
Major guidelines have broadly endorsed a DAPT duration of at least 12 months after PCI as the standard. However, an evolving PCI landscape and continuing research on subgroups have highlighted that standard DAPT may not be optimal for all PCI patients.
Notably, the optimal DAPT duration for HBR patients has remained unclear. The advent of drug-eluting stents (DES) -particularly second-generation DES -and the entry of more potent P2Y12 inhibitors have confounded the problem.
In the increasingly complex HBR arena, clinicians have identified a trend of DAPT outcomes that varies on the duration of the regimen; namely, longer DAPT lowers ischemic risk at the expense of higher bleeding risk, while shorter DAPT reduces bleeding risk but elevates ischemic risk.
Swinging on this pendulum of elevated ischemic or bleeding risk, physicians have leaned on analyzing individual patient characteristics to strike the right balance between the risks and benefits of DAPT.
MASTER DAPT serves as the largest and "first important" randomized trial to report positive results for shorter DAPT in HBR patients, paving the way forward to a new standard of care, according to Gregg W. Stone, MD (Icahn School of Medicine at Mount Sinai, New York, USA).
MASTER DAPT: Key Takeaways
Investigator-initiated, multicenter, randomized, open-label, noninferiority trial
Conducted from February 2017 to December 2019 at 140 sites in 30 countries
- Patient enrollment/characteristics
- Enrollment: 4,579 HBR patients with acute/chronic coronary syndrome undergone successful PCI with biodegradable-polymer sirolimus-eluting stent (Ultimaster, Terumo) (mean age: 76 years; 69.3% men)
- Comorbidities: diabetes 33.6%, chronic kidney disease 18.9%, previous cerebrovascular event 12.4%, peripheral vascular disease 10.6%, concomitant oral anticoagulation 36.4%
- Study design
- 1:1 randomization after PCI (median time from index PCI to randomization: 34 days)
- Randomized to either abbreviated-DAPT (n=2,295) or standard-DAPT (n=2,284)
-
Follow-up data at 335 days for 4,547 patients
- Primary outcomes (abbreviated- vs. standard-DAPT)
- NACE: 7.5% vs. 7.7% (HR 0.97; 95% CI; 0.78-1.20)
(risk difference -0.23%p, 95% CI, -1.80 to 1.33; p<0.001 for noninferiority) - MACCE: 6.1% vs. 5.9% (HR 1.02, 0.80-1.30)
(risk diff. 0.11%p; -1.29 to 1.51; p=0.001 for noninferiority) - Major/clinically relevant nonmajor bleeding: 6.5% vs. 9.4% (HR 0.68, 0.55-0.84)
(risk diff. -2.82%p, -4.40 to -1.24; p<0.001 for superiority)
- NACE: 7.5% vs. 7.7% (HR 0.97; 95% CI; 0.78-1.20)
- Secondary outcomes (abbreviated- vs. standard-DAPT)
- All-cause mortality: 3.3% vs. 3.6% (HR 0.92, 0.67-1.26)
- Myocardial infarction (MI): 2.7% vs. 2.2% (HR 1.22, 0.84-1.78)
- Definite/probable stent thrombosis: 0.6% vs. 0.4% (HR 1.55, 0.67-3.57)
- Cerebrovascular events: 0.8% vs. 1.4% (HR 0.53, 0.29-0.95)
- Stroke: 0.5% vs. 1.0% (HR 0.52, 0.26-1.04)
- BARC type 2 bleeding: 4.5% vs. 6.8% (diff. -2.25%p, -3.59 to -0.90)
- bleeding type 3, 4, 5: 2.3% vs. 2.6%
- BARC type 5 bleeding (fatal): 0.1% vs. 0.4%
- Primary outcomes (abbreviated- vs. standard-DAPT)
Valgimigli stressed that the trial "did not exclude patients with ACS or limit the number, location, or complexity of the treated lesions, unlike other studies" - raising hopes for short DAPT in HBR to maintain ischemic benefits without increasing the risk of adverse clinical events of MI, stroke, major bleeding, and death.
1-month DAPT 'masters' 3 primary outcomes
Although previous studies, such as GLOBAL LEADERS, STOPDAPT-2, ISAR-TRIPLE, DAPT, and PEGASUS-TIMI-54, had examined the safety and efficacy of shorter DAPT, many fell short in suggesting the optimal regimen duration in HBR.
Limitations in study design (i.e., nonrandomization) or strict enrollment criteria such as excluding ACS or complex PCI patients produced inconsistent results that varied according to population characteristics.
Unlike other studies, MASTER DAPT didn’t exclude patients with ACS or limit the number, location, or complexity of treated lesions.
Clinicians have since tailored DAPT duration to the individual patient, while calling for randomized trials that illuminate optimal DAPT for HBR patients.
The investigator-initiated, multicenter, randomized, open-label MASTER DAPT trial honed in on the HBR subgroup and tested the noninferiority of abbreviated-DAPT against standard DAPT in 4,579 patients.
Protocol called for patients in the short-DAPT arm to immediately discontinue DAPT after randomization and continue with single antiplatelet therapy (SAPT) until trial completion. The standard-DAPT arm continued DAPT for 5 additional months (6 months post-PCI) and then continued to antiplatelet monotherapy.
Exceptions were made for patients indicated for oral anticoagulation (OAC). Those on OAC in the short DAPT arm continued SAPT for up to 6 months after PCI. OAC takers in the standard arm continued DAPT for at least 2 additional months (3 months post-PCI).
SAPT consisted of aspirin or a P2Y12 inhibitor, authors noted. Clopidogrel was the most frequently used P2Y12 inhibitor in the standard DAPT group and the most commonly used monotherapy in the abbreviated DAPT group.
The 3 ranked primary outcomes were NACE (composite of death from any cause, MI, stroke, or major bleeding), MACCE (composite of death from any cause, MI or stroke), and major bleeding (BARC type 3, 5) as well as major or clinically relevant nonmajor bleeding (BARC type 2, 3, 5).
Results showed that shorter DAPT, lasting a median of 34 days after PCI, and standard DAPT over a median of 193 days post-PCI showed similar rates of NACE and MACCE.
Shorter DAPT was also superior for major bleeding or clinically relevant nonmajor bleeding outcomes.
Subgroup analysis of MASTER DAPT published in Circulation2 on Aug. 29 on 36% of HBR-PCI patients on OAC versus those not on OAC showed shortening DAPT did not increase ischemic events in patients regardless of OAC administration.
The analysis also showed that BARC 2, 3, or 5 bleeding did not differ significantly with OAC indication, but bleeding rates were lower in the abbreviated DAPT arm not indicated for OAC.
Findings from MASTER-DAPT can be applied directly to a contemporary, real-world setting that includes a diverse group of HBR patients that require DAPT after ACS/PCI
These findings - in line with current recommendations from the 2017 ESC/EACTS guideline and the 2020 ESC guideline for management of ACS in patients without ST-segment elevation for 1- to 6-month DAPT for HBR patients - are expected to ramp up the weak strength of the endorsement (LoE: C) that currently only reflects the opinion for task force members.
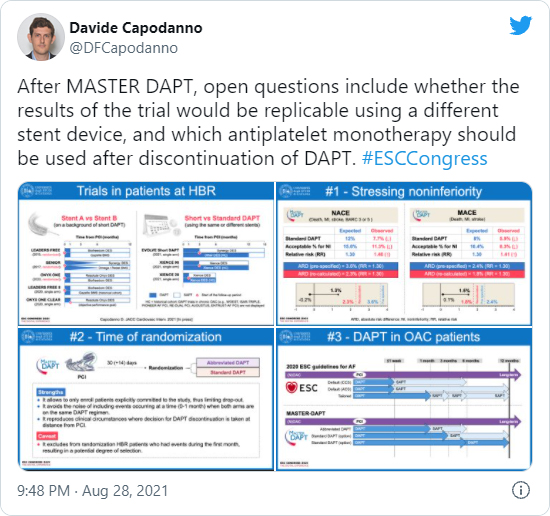
Pursuing discussion at ESC 2021and on Twitter asked whether the "game-changing" results could be applied to different stent devices and questioned the choice of SAPT after discontinuing DAPT.
In an accompanying editorial3, Erik Magnus Ohman, MD (Duke University School of Medicine, North Carolina, USA) welcomed the important findings for HBR patients that represent a “major shift” that “moves toward a shorter and simpler antithrombotic strategy after PCI, with concomitant shorter antiplatelet monotherapy for chronic disease after DES implantation.”
However, Ohman also cautioned that the use of abbreviated DAPT may be reasonable only in the context of the Ultimaster DES stent used in the trial, and may not be applicable to later-generation DES.
The noninferiority design also represents some challenges in interpreting study findings and determining an acceptable trade-off that supports shorter DAPT. For instance, although composite ischemic outcome showed noninferiority, the wide 95% CI for HR encompassed a potential 30% higher incidence in the short DAPT arm, which is “higher than some would consider to be a reasonable trade-off between bleeding and ischemic events.”
The wide confidence interval in MASTER DAPT, Ohman added, pales to the “tighter and relative” boundaries for noninferiority in previous trials, thereby calling for additional trials to replicate findings.
Until further trials help clear ambiguity from the HBR realm, many emphasized the wide applicability of MASTER-DAPT findings.
Duk-Woo Park, MD (Asan Medical Center, Seoul, South Korea) summarized findings and commented to SummitMD that: “The MASTER-DAPT trial demonstrated abbreviated 1-month DAPT may be optimal for safety and efficacy for HBR patients who had undergone implantation with a biodegradable polymer sirolimus-eluting stent for ACS for NACE, MACCE, and bleeding endpoints compared to 3-month DAPT. Findings from this trial can be directly applied to contemporary, real-world clinical practice, which is known for having a wide range of HBR patients who require DAPT after ACS or PCI.”
Edited by

Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
Written by


Leave a comment