News | SummitMD
OCTIVUS Trial Subgroup Analysis for Complex Coronary Lesions Revealed at TCT 2023
Promising Findings Yet Hypothesis-Generating: Acknowledging Limitations and the Call for Further Research
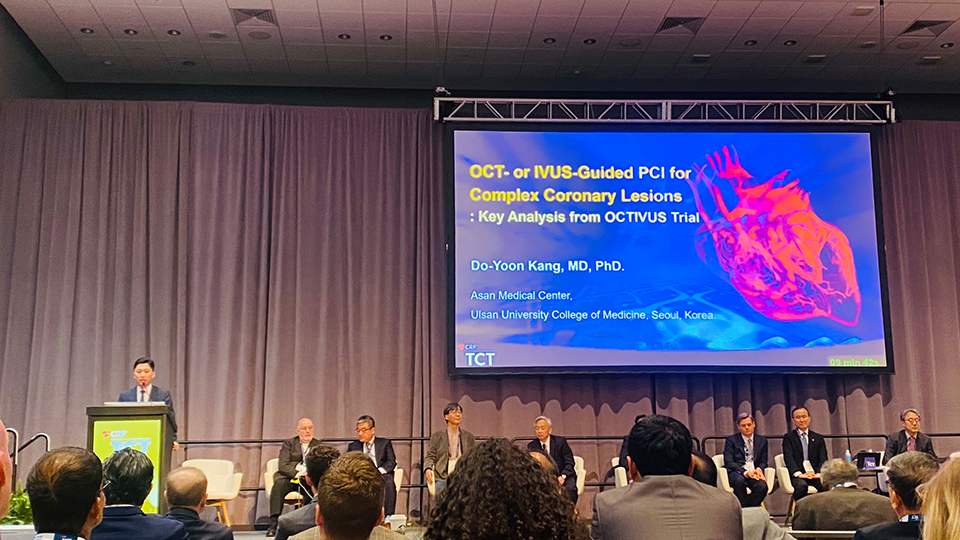
Do-Yoon Kang, MD, PhD (Asan Medical Center) presented the Key Analysis from the OCTIVUS Trial during the 35th TCT 2023 held at the Moscone Center in San Francisco, CA on October 23.
At the TCT WorldLink East Asia Featured Clinical Science, Dr. Do-Yoon Kang unveiled pivotal findings from the key subgroup analysis of the OCTIVUS trial for the treatment of complex coronary artery lesions.
The OCTIVUS trial was a prospective, multi-center, randomized, open-label trial that compared Optical Coherence Tomography (OCT) and Intravascular Ultrasound (IVUS) in guiding Percutaneous Coronary Interventions (PCI) in a total of 2008 patients. Of those, this study compared OCT-guided PCI with IVUS-guided PCI in patients with complex coronary lesions in 1475 patients, including unprotected left main disease, bifurcation disease, aorto-ostial lesions, chronic total occlusions, severely calcified lesions, in-stent restenosis, diffuse long lesions, and multivessel disease. Dr. Kang highlighted the use of Cox proportional hazards models and overlap propensity-score weighting to adjust patient characteristics and reduce treatment selection bias.
The mean age was about 65 years, and 21% were women. Lesion characteristics were similar in the two groups, although there was a lower proportion of left main disease and a lower mean SYNTAX score in the OCT group. Contrast dye used was greater, and total PCI time was shorter in the OCT-guided group. There was no difference in the rate of contrast-induced nephropathy between the two groups, but major procedural complications requiring intervention were less frequent in the OCT group (1.7% vs 3.4%; P = 0.03). The imaging devices showed no complications throughout the course of the study.
Key findings revealed that OCT-guided PCI showed comparability to IVUS with the primary endpoint of a composite of cardiac death, target-vessel myocardial infarction (MI), or target-vessel revascularization over a median follow-up of 2 years (6.5% in the OCT group vs. 7.4% in the IVUS group; HR 0.87; 95% CI 0.59-1.29). The results remained steadfastly consistent between the groups, even after adjustments.
Most secondary endpoints occurred at similar rates in the two groups, except that target-vessel MI was less common in the OCT group (0.8% vs 2.4%; P = 0.03).
In subgroup analyses by lesion type, results were generally the same as in the overall analysis, except that in patients treated for in-stent restenosis, OCT guidance was associated with a lower rate of target vessel failure compared with IVUS guidance (10.5% vs 29.5%; HR 0.36; 95% CI 0.17-0.78).
While presenting the findings, Dr. Kang astutely underscored the imperative of acknowledging the inherent constraints of the study. The number of primary-outcome events was lower than expected, and the impossibility of masking imaging modalities from patients and investigators could introduce bias. Additionally, he noted the potential for discrepancies in site-determined and core-laboratory measured imaging interpretation.
In patients with complex coronary lesions, Dr. Kang formulated the following conclusions, OCT-guided PCI showed a similar risk of a composite of death from cardiac causes, target-vessel MI, or ischemia-driven target-vessel revascularization compared to IVUS-guided PCI during the median 2-year follow-up.
However, owing to insufficient statistical power and inherent limitations from subgroup analysis, the overall finding should be hypothesis-generating, and further research is needed in this area.
Edited by

Hoyun Kim, MD
Sejong Hospital, Korea (Republic of)

KyungAe Kim, RN
CardioVascular Research Foundation (CVRF), Korea (Republic of)
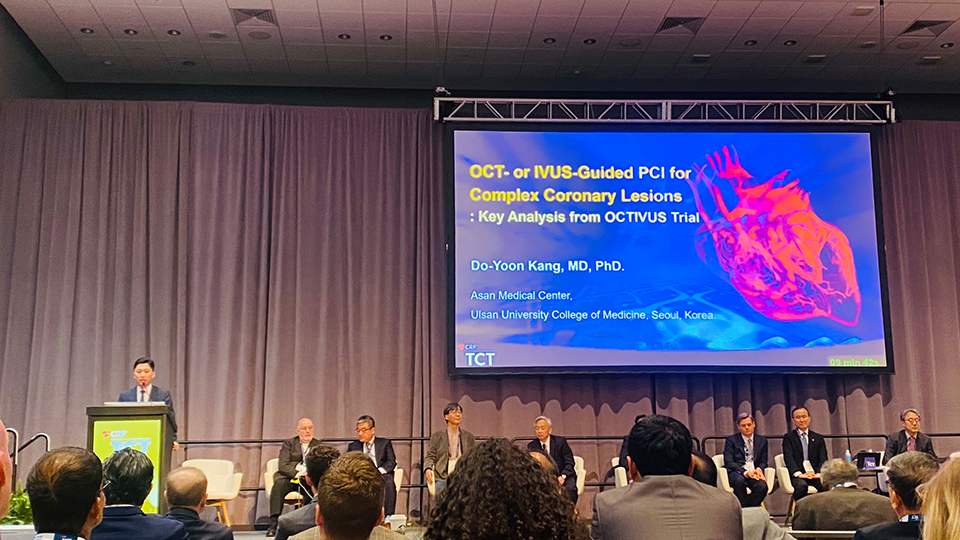
Do-Yoon Kang, MD, PhD (Asan Medical Center) presented the Key Analysis from the OCTIVUS Trial during the 35th TCT 2023 held at the Moscone Center in San Francisco, CA on October 23.
At the TCT WorldLink East Asia Featured Clinical Science, Dr. Do-Yoon Kang unveiled pivotal findings from the key subgroup analysis of the OCTIVUS trial for the treatment of complex coronary artery lesions.
The OCTIVUS trial was a prospective, multi-center, randomized, open-label trial that compared Optical Coherence Tomography (OCT) and Intravascular Ultrasound (IVUS) in guiding Percutaneous Coronary Interventions (PCI) in a total of 2008 patients. Of those, this study compared OCT-guided PCI with IVUS-guided PCI in patients with complex coronary lesions in 1475 patients, including unprotected left main disease, bifurcation disease, aorto-ostial lesions, chronic total occlusions, severely calcified lesions, in-stent restenosis, diffuse long lesions, and multivessel disease. Dr. Kang highlighted the use of Cox proportional hazards models and overlap propensity-score weighting to adjust patient characteristics and reduce treatment selection bias.
The mean age was about 65 years, and 21% were women. Lesion characteristics were similar in the two groups, although there was a lower proportion of left main disease and a lower mean SYNTAX score in the OCT group. Contrast dye used was greater, and total PCI time was shorter in the OCT-guided group. There was no difference in the rate of contrast-induced nephropathy between the two groups, but major procedural complications requiring intervention were less frequent in the OCT group (1.7% vs 3.4%; P = 0.03). The imaging devices showed no complications throughout the course of the study.
Key findings revealed that OCT-guided PCI showed comparability to IVUS with the primary endpoint of a composite of cardiac death, target-vessel myocardial infarction (MI), or target-vessel revascularization over a median follow-up of 2 years (6.5% in the OCT group vs. 7.4% in the IVUS group; HR 0.87; 95% CI 0.59-1.29). The results remained steadfastly consistent between the groups, even after adjustments.
Most secondary endpoints occurred at similar rates in the two groups, except that target-vessel MI was less common in the OCT group (0.8% vs 2.4%; P = 0.03).
In subgroup analyses by lesion type, results were generally the same as in the overall analysis, except that in patients treated for in-stent restenosis, OCT guidance was associated with a lower rate of target vessel failure compared with IVUS guidance (10.5% vs 29.5%; HR 0.36; 95% CI 0.17-0.78).
While presenting the findings, Dr. Kang astutely underscored the imperative of acknowledging the inherent constraints of the study. The number of primary-outcome events was lower than expected, and the impossibility of masking imaging modalities from patients and investigators could introduce bias. Additionally, he noted the potential for discrepancies in site-determined and core-laboratory measured imaging interpretation.
In patients with complex coronary lesions, Dr. Kang formulated the following conclusions, OCT-guided PCI showed a similar risk of a composite of death from cardiac causes, target-vessel MI, or ischemia-driven target-vessel revascularization compared to IVUS-guided PCI during the median 2-year follow-up.
However, owing to insufficient statistical power and inherent limitations from subgroup analysis, the overall finding should be hypothesis-generating, and further research is needed in this area.
Edited by

Hoyun Kim, MD
Sejong Hospital, Korea (Republic of)

KyungAe Kim, RN
CardioVascular Research Foundation (CVRF), Korea (Republic of)

Leave a comment