News | TCTAP 2024
FFR and iFR: Where Do We Stand Today?
Coronary Physiology: New Insights

Nico Pijls
Catharina Hospital, Netherlands
Reassessment of Coronary Artery Disease Diagnostics: FFR Reigns Supreme
In the evolving landscape of cardiology, the debate over the most reliable method for assessing coronary artery disease has reached a crucial juncture. Fractional Flow Reserve (FFR) and Instantaneous Wave-free Ratio (iFR) have both been subjects of intense scrutiny and discussion. However, recent insights, especially new recommendations from leading cardiology journals and associations, are reaffirming FFR as the gold standard for assessing coronary artery disease.
Understanding FFR and iFR
FFR is an index that measures the maximum achievable blood flow in the presence of a coronary stenosis compared to normal maximum flow. The underlying principles of FFR are rooted in sound physiology. It evaluates the functional capacity of a patient's heart under maximum vasodilation, correlating to exercise tolerance. This method has significantly influenced decision-making in catheterization labs, aiding in precise revascularization strategies and improving patient outcomes. However, FFR measurement necessitates a pharmacological hyperemic stimulus, typically involving adenosine or ATP infusion. Although these agents have transient side effects, the benefits of accurate measurement outweigh the minor inconveniences.
In contrast, iFR emerged as a simpler alternative to FFR. Proposed by Davies et al., iFR measures the resting Pd/Pa ratio during a specific part of diastole, eliminating the need for a hyperemic stimulus. Initial enthusiasm for iFR was bolstered by two large randomized controlled trials (DEFINE-FLAIR and SWEDE-HEART), which suggested non-inferiority of iFR compared to FFR.
Critical Analysis of iFR
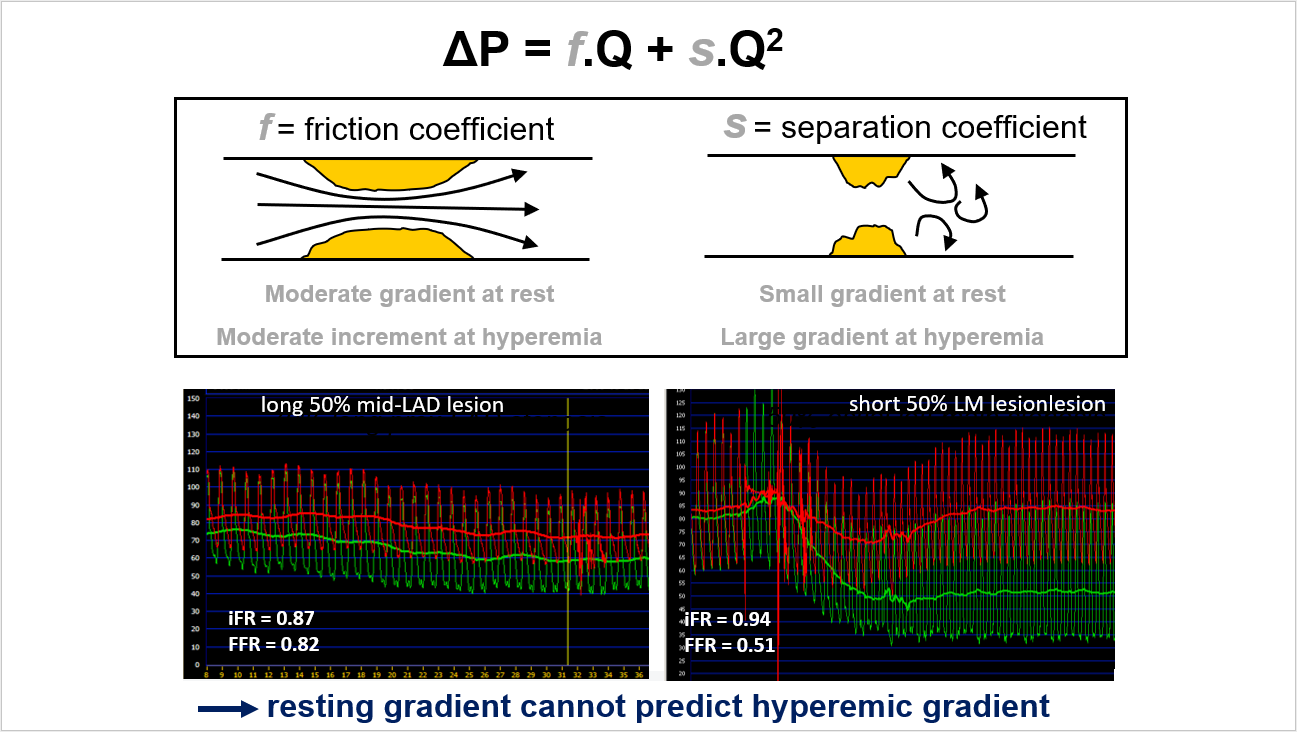
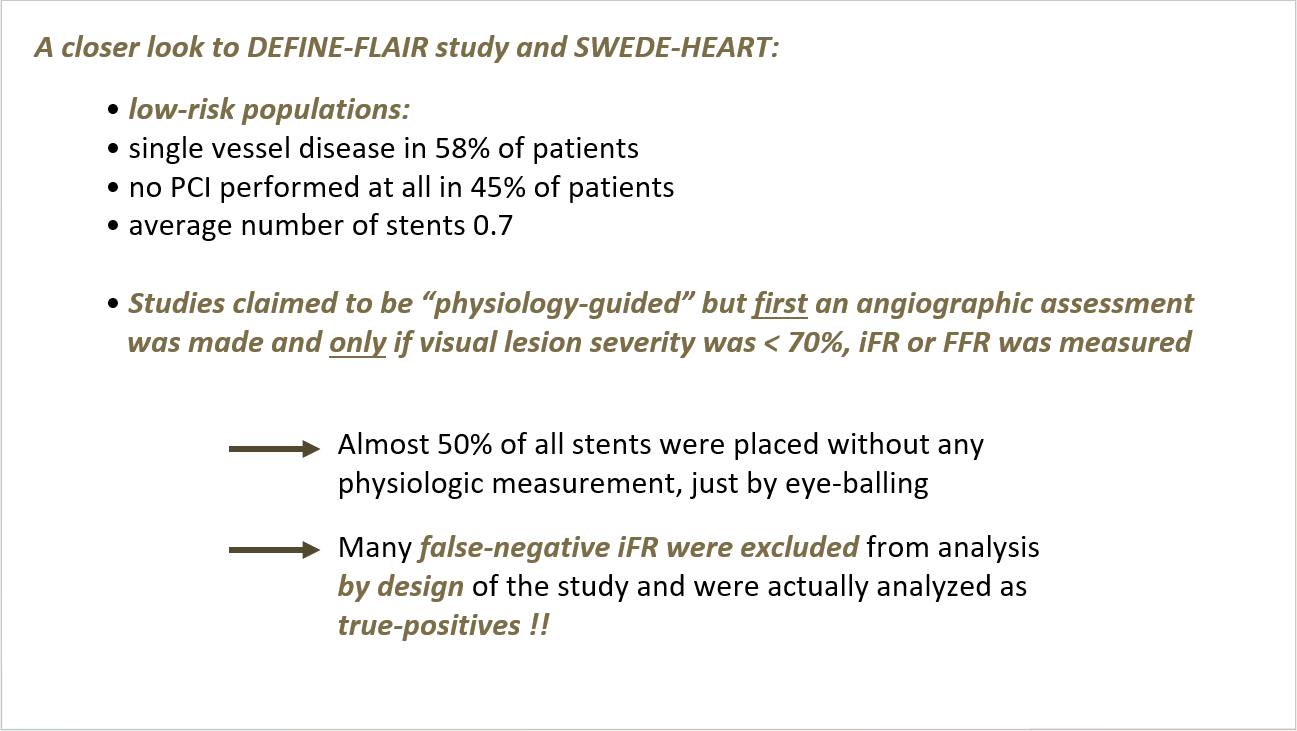
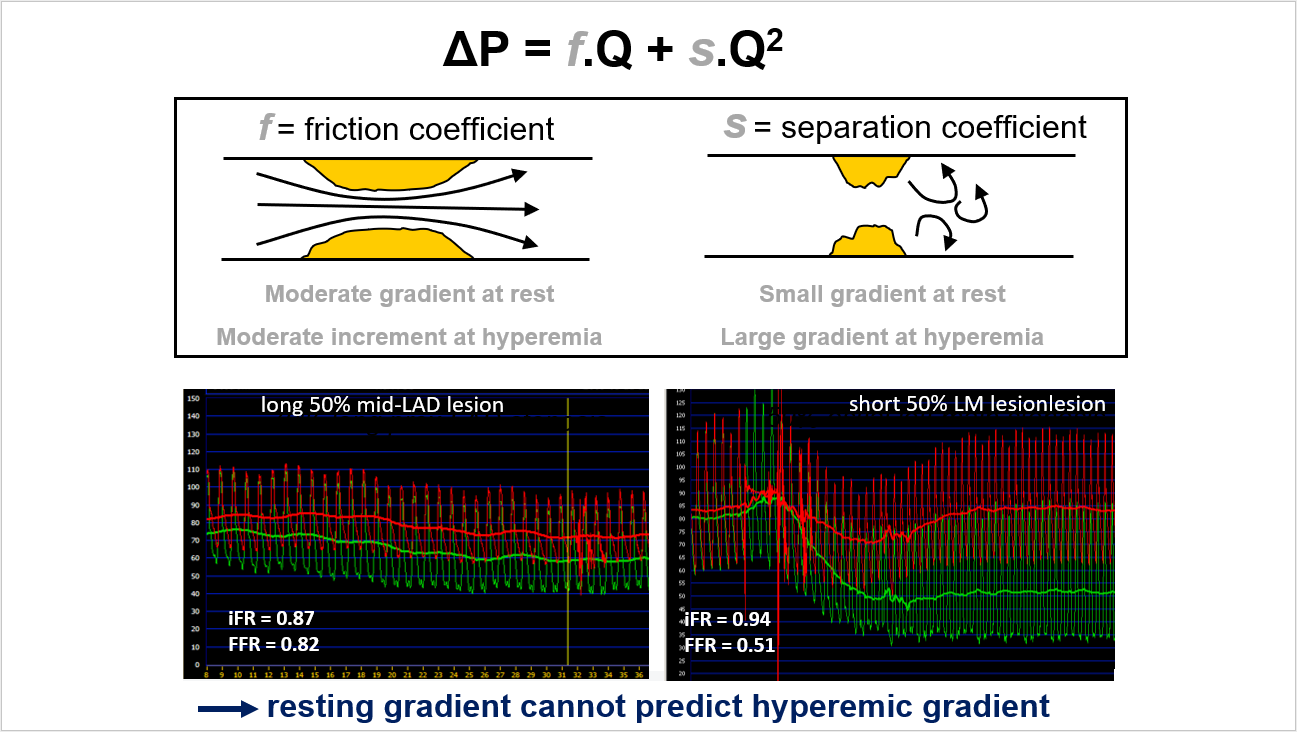
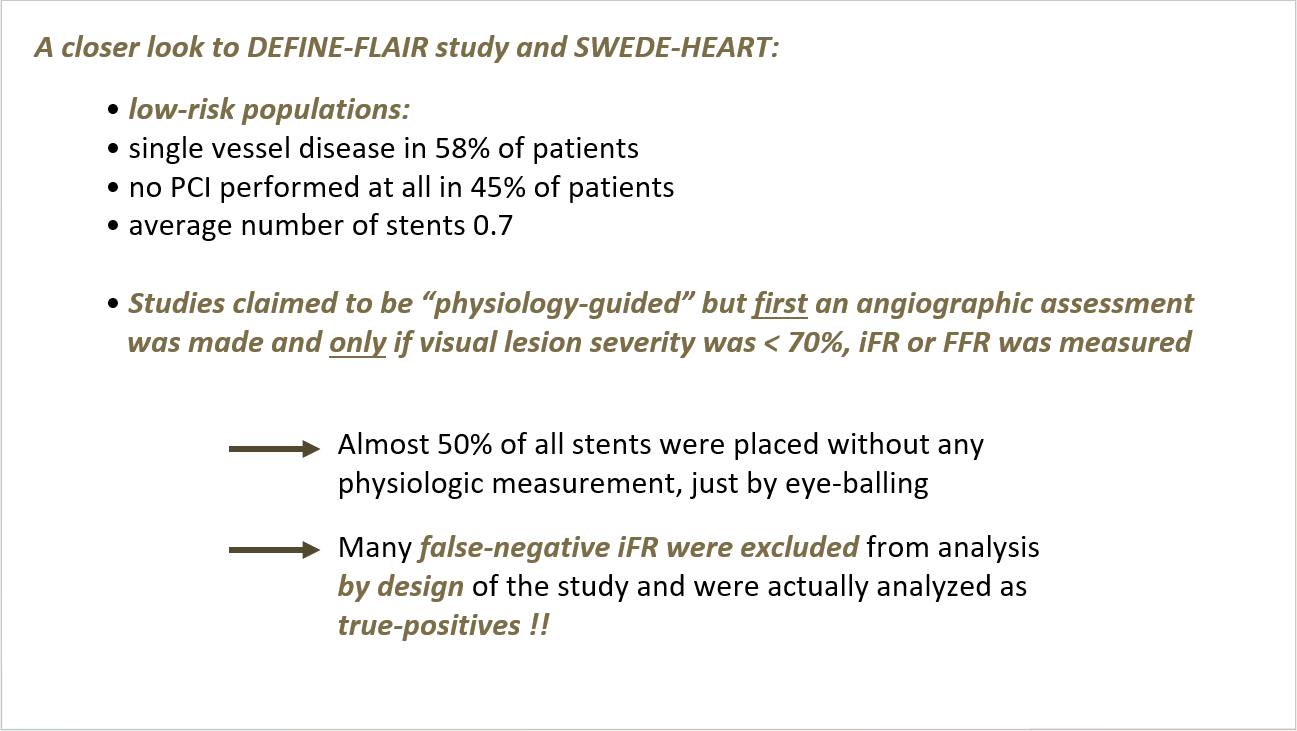
Despite the initial optimism, several concerns about iFR have come to light. The concept of a “wave-free period” during diastole lacks a solid physiological basis, and predicting hyperemic gradients from resting gradients has proven unreliable. Furthermore, serious design and interpretation issues in the DEFINE-FLAIR and SWEDE-HEART studies have raised questions about their validity. Notably, these studies involved low-risk populations, with a significant proportion of patients not undergoing PCI and many stents placed without physiological measurements.
Biases in the study designs were particularly problematic. For example, almost 50% of stents were placed based on visual lesion severity rather than physiological measurement. Many false-negative iFR results were excluded from the analysis, skewing the data to appear more favorable. This bias went largely unrecognized by investigators, leading journals, and guideline committees.
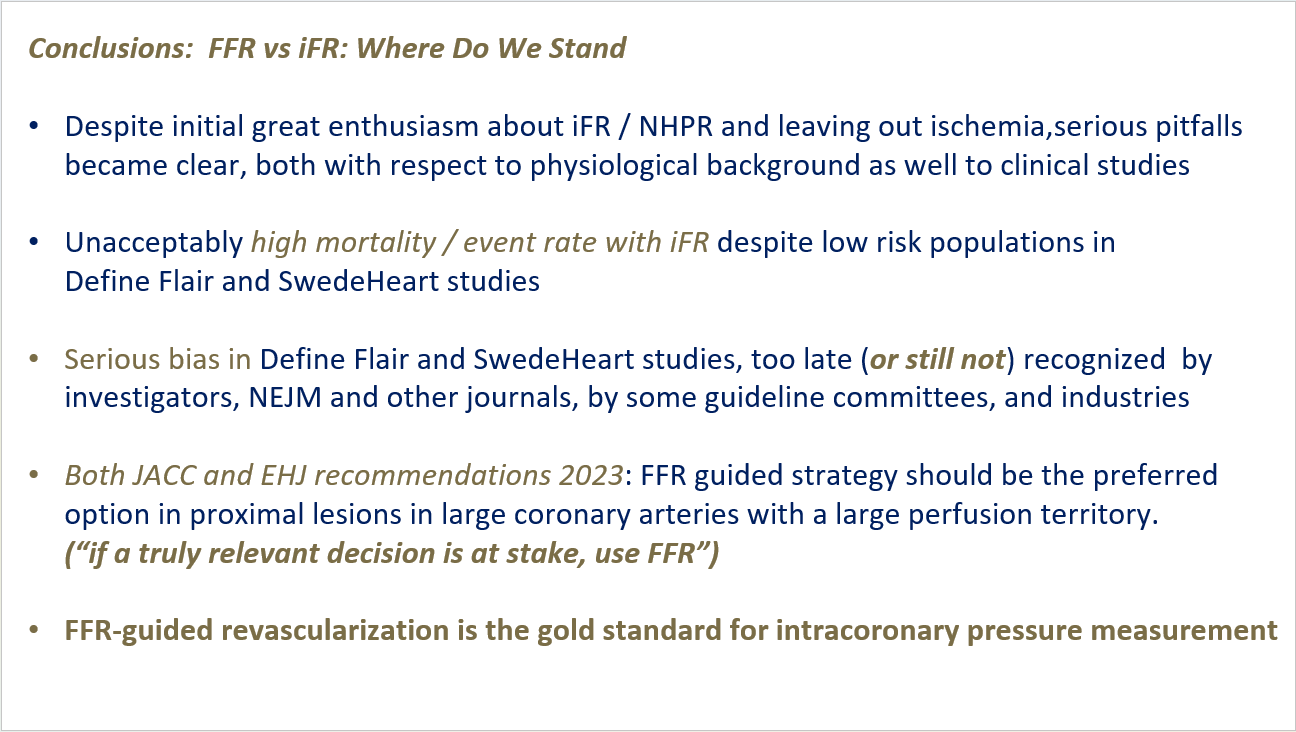
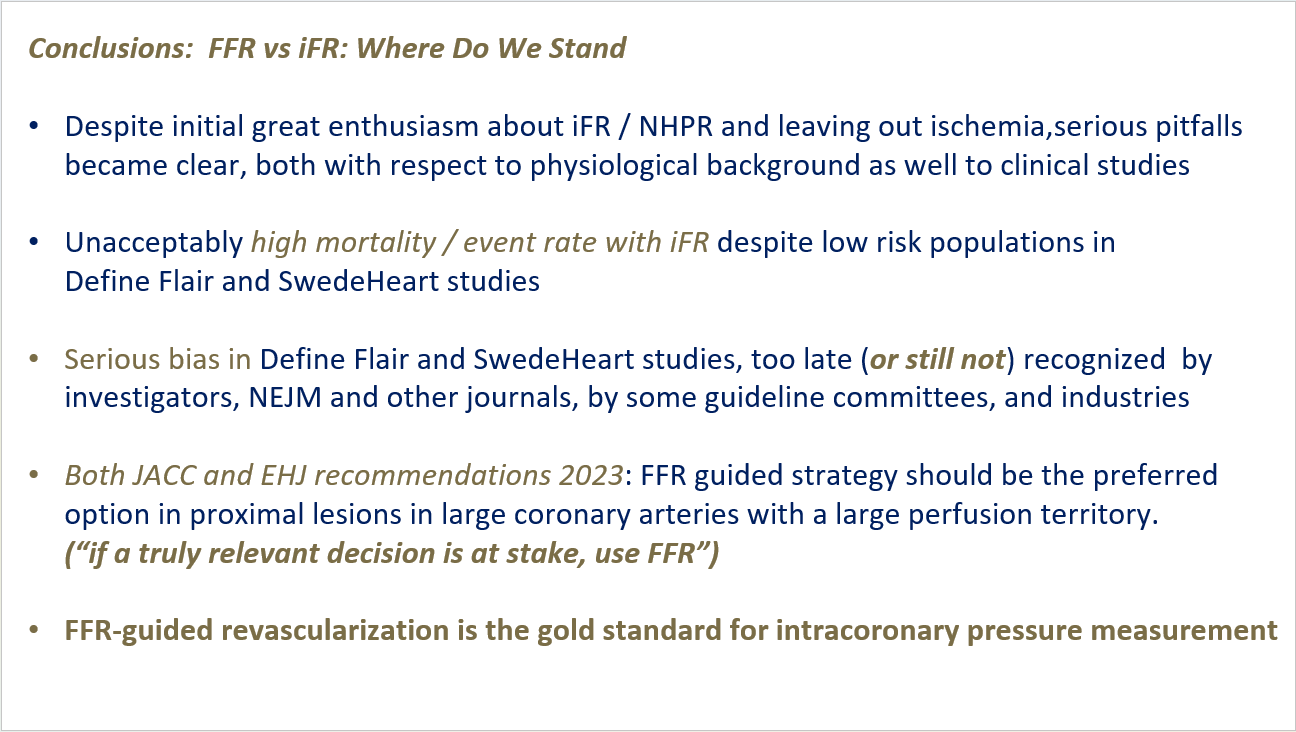
Long-term follow-ups revealed troubling outcomes. Mortality rates in the iFR-guided groups were significantly higher than those in FFR-guided groups, a disparity that increased over time. These findings have prompted a reassessment of iFR's reliability, especially in high-stakes clinical decisions.
New Recommendations
In response to these revelations, the Journal of the American College of Cardiology (JACC) and the European Heart Journal (EHJ) now recommend FFR as the preferred method for assessing proximal lesions in large coronary arteries. Upcoming guidelines are expected to reflect this preference, emphasizing FFR-guided revascularization as the standard for intracoronary pressure measurement.
The cardiology community's initial enthusiasm for iFR and other non-hyperemic pressure ratios has been tempered by emerging evidence of their limitations. The biases and higher mortality rates observed in key studies underscore the necessity of relying on methods with a robust physiological basis. As such, FFR remains the gold standard, ensuring precise diagnostics and optimal patient outcomes in coronary artery disease management.
Hot Topics
Coronary Physiology: New Insights
Friday, April 26, 3:30 PM ~ 5:44 PM
Presentation Room 2, Level 1
Edited by

Yeong Jin Jeong, MD
Sarang General Hospital, Korea (Republic of)

Nico Pijls
Catharina Hospital, Netherlands
Reassessment of Coronary Artery Disease Diagnostics: FFR Reigns Supreme
In the evolving landscape of cardiology, the debate over the most reliable method for assessing coronary artery disease has reached a crucial juncture. Fractional Flow Reserve (FFR) and Instantaneous Wave-free Ratio (iFR) have both been subjects of intense scrutiny and discussion. However, recent insights, especially new recommendations from leading cardiology journals and associations, are reaffirming FFR as the gold standard for assessing coronary artery disease.
Understanding FFR and iFR
FFR is an index that measures the maximum achievable blood flow in the presence of a coronary stenosis compared to normal maximum flow. The underlying principles of FFR are rooted in sound physiology. It evaluates the functional capacity of a patient's heart under maximum vasodilation, correlating to exercise tolerance. This method has significantly influenced decision-making in catheterization labs, aiding in precise revascularization strategies and improving patient outcomes. However, FFR measurement necessitates a pharmacological hyperemic stimulus, typically involving adenosine or ATP infusion. Although these agents have transient side effects, the benefits of accurate measurement outweigh the minor inconveniences.
In contrast, iFR emerged as a simpler alternative to FFR. Proposed by Davies et al., iFR measures the resting Pd/Pa ratio during a specific part of diastole, eliminating the need for a hyperemic stimulus. Initial enthusiasm for iFR was bolstered by two large randomized controlled trials (DEFINE-FLAIR and SWEDE-HEART), which suggested non-inferiority of iFR compared to FFR.
Critical Analysis of iFR
Despite the initial optimism, several concerns about iFR have come to light. The concept of a “wave-free period” during diastole lacks a solid physiological basis, and predicting hyperemic gradients from resting gradients has proven unreliable. Furthermore, serious design and interpretation issues in the DEFINE-FLAIR and SWEDE-HEART studies have raised questions about their validity. Notably, these studies involved low-risk populations, with a significant proportion of patients not undergoing PCI and many stents placed without physiological measurements.
Biases in the study designs were particularly problematic. For example, almost 50% of stents were placed based on visual lesion severity rather than physiological measurement. Many false-negative iFR results were excluded from the analysis, skewing the data to appear more favorable. This bias went largely unrecognized by investigators, leading journals, and guideline committees.
Long-term follow-ups revealed troubling outcomes. Mortality rates in the iFR-guided groups were significantly higher than those in FFR-guided groups, a disparity that increased over time. These findings have prompted a reassessment of iFR's reliability, especially in high-stakes clinical decisions.
New Recommendations
In response to these revelations, the Journal of the American College of Cardiology (JACC) and the European Heart Journal (EHJ) now recommend FFR as the preferred method for assessing proximal lesions in large coronary arteries. Upcoming guidelines are expected to reflect this preference, emphasizing FFR-guided revascularization as the standard for intracoronary pressure measurement.
The cardiology community's initial enthusiasm for iFR and other non-hyperemic pressure ratios has been tempered by emerging evidence of their limitations. The biases and higher mortality rates observed in key studies underscore the necessity of relying on methods with a robust physiological basis. As such, FFR remains the gold standard, ensuring precise diagnostics and optimal patient outcomes in coronary artery disease management.
Hot Topics
Coronary Physiology: New Insights
Friday, April 26, 3:30 PM ~ 5:44 PM
Presentation Room 2, Level 1
Edited by

Yeong Jin Jeong, MD
Sarang General Hospital, Korea (Republic of)

Leave a comment